Dr Drew Weissman had dreamed about the seemingly endless possibilities of treating diseases with custom-made mRNA. However, he didn’t expect the mRNA technology he co-created with former colleague Katalin (Kati) Karikó to become critical to some of the Covid-19 mRNA-based vaccines and win them a Nobel Prize.
In an interaction with THE WEEK, done in the midst of the pandemic, Weissman shared the science behind mRNA and his journey to creating the mRNA vaccine technology that is a critical component of Pfizer-BioNTech’s and Moderna’s mRNA-based Covid-19 vaccines and others being developed globally. Excerpts:
Before we discuss the vaccines, could you shed some light on what is the role of mRNA and DNA?
Sure. The way our cell and our body works is that our DNA contains all of our genetic information. Every protein in our body is coded for in the DNA. The way the body makes a protein from that DNA is that it uses an mRNA―a messenger RNA. So, an enzyme copies protein off the DNA, the mRNA then travels to a machine called a ribosome. But it is essentially a machine that can read the code in the mRNA and turn that into a protein. So, it is kind of a middleman. It is in between the DNA and the protein. It is responsible for making proteins in a cell. So, the way the mRNA vaccine works is that we encode the spike protein from coronavirus as an mRNA. We give it to a cell and the ribosomes; the cell machines read the mRNA and produce the spike protein. The body then recognises that spike protein as foreign and makes an immune response against it.
You have been working on the mRNA vaccine for a few years. Could you give us a little bit of history of the vaccine journey?
I came to UPenn 23 years ago and met Kati Karikó at a copy machine. I have studied vaccines and she studied mRNA but wasn't getting very far and nobody in the mRNA field was advancing. So, we started to investigate mRNA in the immune system, and we figured out that mRNA was highly inflammatory and that was problematic. Because if you give mRNA to a patient, you don't want to get sick from it. So, we figured out what made it so inflammatory and then we figured out how to avoid that inflammation and that was our breakthrough in 2005. It is called nucleoside modified mRNA. And what we essentially did was we changed the mRNA, so that the immune system in our bodies did not recognise it as foreign. And that is the mRNA that is used in the Moderna and Pfizer-BioNTech vaccines.
Do you think mRNA manipulation is a holy grail for other diseases as well?
I think the therapeutic platform has enormous potential. It has worked unbelievably well for Covid in the hands of two different companies. We are doing clinical trials for five more pathogens right now. BioNTech and Moderna are doing additional clinical trials. mRNA vaccines are in phase 2 clinical trials for cancer as personalised vaccines and have shown great success or better success so far. It has enormous potential and my guess is that it is going to be a turning point in medicine, but you will have to see.
Do you think mRNA vaccines have an advantage over other type of vaccines? If so, what are some of these that we are seeing for Covid-19?
The two mRNA vaccines from Moderna and Pfizer are the first ones licensed. So, this is the first comparison that we have got. It is hard to say whether they are better or have advantages [over other vaccines]. What we do know is one of their advantages is that they are incredibly quick to make. So, if you have to make an inactivated virus vaccine, that is a lot of work. You have to figure out how to grow the virus, how to inactivate it, how to purify it, how to make sure it is safe. With mRNA you only need the sequence of the protein of interest. So for coronavirus, that is the spike protein and we have known for over 20 years that the spike protein is the principal vaccine component. The day that this sequence was released, we made an mRNA vaccine for it. So it is very quick. It is also very effective. We have seen that in the clinical trials and in the patients―[it had] 90-95 per cent efficacy against any symptoms and 100 per cent efficacy against serious symptoms and death. There are a lot of unknowns still and we will learn those over time.
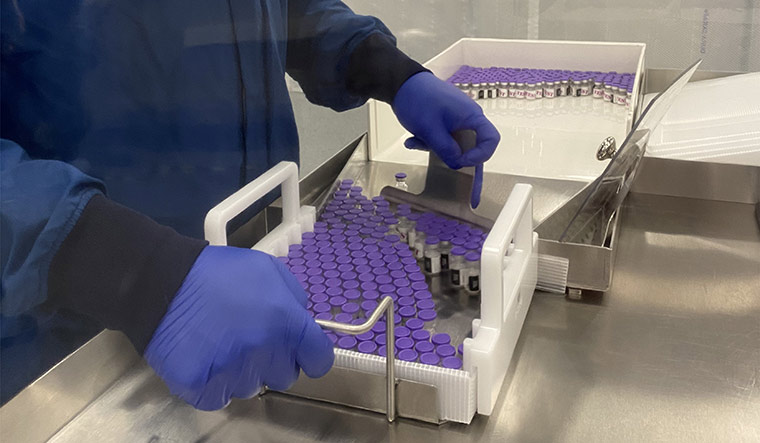 Viral and vial: An employee at the Pfizer manufacturing facility in Kalamazoo, Michigan, during Covid-19 | Reuters
Viral and vial: An employee at the Pfizer manufacturing facility in Kalamazoo, Michigan, during Covid-19 | Reuters
Is there a difference in the antibody repertoire between mRNA-based vaccines and attenuated virus vaccines?
There are a couple of differences and this has not been investigated well yet. We have investigated in animal models and what we see is that mRNA vaccines give much higher levels. Even in the phase 3 trials, the level of antibodies in vaccinated people were about five times higher than convalescent patients. With other vaccines, the antidotes typically give a level similar to the convalescent patients. So the mRNA vaccines make higher levels of antibodies. As part of that, some of those antibodies neutralise the virus―kill the virus before it can infect a cell―those levels are also higher. We are looking at specificities. So, particular parts of the spike that the vaccines can recognise, and we have identified some that mRNA induces well, that infection doesn't induce and some of those are conserved antigens that may offer broad protection. Those are new and ongoing studies. In general, the mRNA vaccines are better than most other vaccines. They give higher levels of antibodies.
These vaccines are all against the spike protein and when we are using mRNA, you're using a discrete region of the spike protein versus the traditional method where you are using potentially a larger segment. So, are there regions of the spike protein, for instance, which are less subject to mutation, which would be better targets?
Another thing that my lab is doing is we have been working on a pan-coronavirus vaccine and what that means is that there have been three coronavirus epidemics in the past 20 years. It would be foolish to not think that we are going to have more. We are definitely going to have more coronavirus epidemics and potential pandemics in the future. What we started doing last summer is try to make a vaccine that would prevent or protect against any bad coronaviruses that have the potential to infect humans. The way we are doing that is we are looking at conserved regions of the entire virus as well as conserved regions of the spike protein, and we are trying to make vaccines that induce those responses. We had some success; we have made a vaccine that can prevent SARS, which was the first coronavirus we know about, and Covid-19 as well. So it looks like we have the potential to make a pan-coronavirus vaccine. But you are right―it is identifying the right immunogens, the right regions of the spike protein and the entire virus to use in a vaccine.
What do we know about the duration of action of the immune response?
Right now, Moderna and Pfizer-BioNTech are measuring antibody levels over time. We can predict that in a year, [vaccinated people] will probably be well protected, but we don't know if the vaccine is going to last a year, five years, 10 years. The other issue is that a vaccine does two things―it makes memory and it makes effector, which are active antibodies and T-cells. They are only measuring active antibodies in the blood. There are memory B cells that respond very quickly. And for all we know you could have zero antibodies in your blood. But if you have got good memory cells, you will make a response fast enough and you are completely protected. So, it is really going to be about following people over time and seeing when they start getting the disease again, and that will tell us when the vaccine needs to be boosted.
Why do we need multiple shots to make mRNA vaccines create more antibodies? Why is there a more pronounced reaction after multiple shots? And what is shown about delaying the booster dose?
Those are great questions, but we don't have answers to all of them. We have developed probably over 30 different vaccines using mRNA for everything, from Zika to Ebola to genital herpes, HIV, influenza, hepatitis C. Some of those vaccines work well with a single injection, others require multiple. If you look at the phase 3 trials, both the Moderna and the Pfizer vaccines are 80 per cent effective after a single [dose]. What we don't know and what the concern was was that how durable that response is and that gets into basic immunology. And in basic immunology, the first time you see a pathogen or an antigen, the response is limited and it is usually not very potent and the immune system requires a boost, a second vision of that pathogen to make a better response. And that is why most vaccines are given two, three, four times to boost and to improve the response. We see the same thing with mRNA, the level of antibodies goes up about 10 to 20-fold when somebody gets a booster. And that is why you go from 80 per cent to 95 per cent protection. We are now investigating the effect on longevity. Nobody or very few people got a single vaccine with the mRNA. So, it is going to be hard to know [whether] one vaccine dose will give you years of protection. But people wanted 95 per cent protection and good durability and that is why they get two doses.
 Testing times: A file photo of a man getting vaccinated in Bengaluru | Bhanu Prakash Chandra
Testing times: A file photo of a man getting vaccinated in Bengaluru | Bhanu Prakash Chandra
What about booster dose side-effects? I felt a little lousy, a couple friends of mine felt terrible. Some others were very sick. Is there any data on these second dose side-effects? Or, is this just a case of immune systems being funny and individualised?
If you look at the side effects, 80 to 90 per cent of people get sore arms, swelling at the site and a smaller percentage gets systemic effects. This is telling us that the vaccines are working. This is the immune system responding to the vaccine. It has nothing to do with manufacturing. It has nothing to do with contaminants or any other problems with the vaccine. They appear to be purely our immune system responding. In my mind, it is a good thing if you have an adverse event because it means the vaccine is doing its job. Having said that, we are working on newer vaccines that have fewer of these adverse events, so that the vaccine is better tolerated.
My friend has some familiar arthritis in his carpometacarpal joints, at the base of his thumb. And he seemed to have gotten some severe arthritic flare-ups within 12 hours of his second shot. Is this the sort of thing that you might expect when the immune system gets amped up from that second/booster shot?
Yeah, we just don’t know. I mean look at the vaccines in the phase 3 clinical trials. People with arthritis and autoimmune diseases weren't included in those trials. There is no scientific evidence from any animal studies or earlier human trials that the vaccines will cause a flare up in an autoimmune disease. But that's not to say it may not happen when your immune system is amped up… there is a potential that it will recognise other antigens, autoantigens that it regularly recognises. So this is something that needs to be studied.
As far as we know at this point, are mRNA vaccines less effective on cancer patients or even more specifically blood cancer patients?
Certainly, for anybody with an impaired immune system, the vaccine is not going to work as well. If anybody has had their B-cells depleted with CD19 antibodies or CD19 Car T's, they are not expected to make much of an antibody response. They will still make some T-cell response which offers some protection. We don't have good data yet, but the more immunosuppressed the person is, the less well they are going to respond to a vaccine.
How effective do you think mRNA vaccines would be against newer variants of Covid-19?
What we know so far is that the mRNA vaccines still appear to be effective against all other variants so far. What we don't know is what is going to show up in the future…. So, the concern is that in the future a variant might appear that the vaccine is completely useless against. For mRNA vaccines, it is very simple to make an update―a booster and improvement. I was talking to the person who runs BioNTech who said it would take them six weeks to have a new vaccine in a patient's arms. So mRNA allows you to very quickly update vaccines, which I suspect will be important as new variants appear.
Priya Menon produces and hosts CureTalks, an internet talk show on health care. She works as Vice President, TrialX, a clinical trial solutions company headquartered in New York.



