It is 2am in southern Minnesota. Physician Priya Sampathkumar is up coordinating with friends to find oxygen for a Covid-19 patient she has never met, back in India. She manages to find an oxygen concentrator and, via Facetime with the patient’s caregiver, provides instructions on how to use it. While others sleep, she works into the wee hours from her Rochester home to help random strangers who reach out to her via her Twitter feed asking for help.
As the Covid-19 situation in India worsened, she took leave of absence from her duties as chair of infection prevention and control, and infectious disease specialist, Mayo Clinic, Minnesota, to help out as many people as possible. She said she was heartbroken by the Covid-19 situation in India. “I have family in different parts of India. I cannot eat or sleep, I am so worried,” she said. “I am still seeing wedding invitations and party invitations going around in the India groups. Why aren’t people taking the situation seriously?” She emphasised that behaviour would have to change for us to truly overcome the challenge of the pandemic.
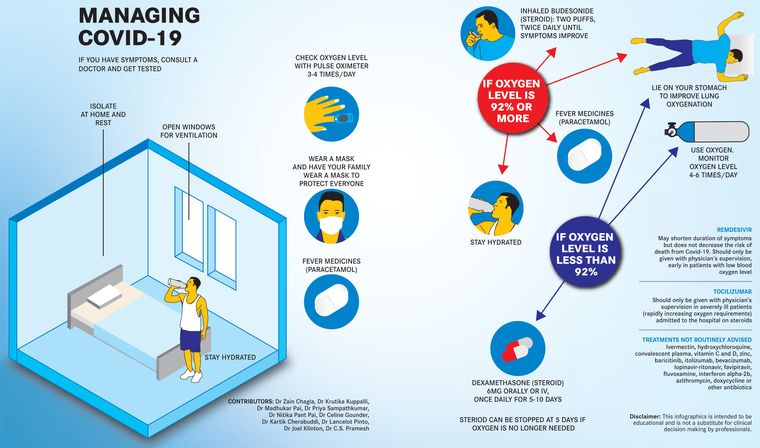
Sampathkumar, and her husband Dr Vincent Rajkumar, also working at Mayo Clinic, Minnesota, are part of the India Covid SOS, an international group aimed at “sharing evidence-based solutions” to mitigate the crisis (see infographics on pages: 28-31). During an hour-long discussion, she speaks about the gaps that may have caused the proportions of Covid cases in India. She mentions the requirement for sending out correct public messages on prevention, control, treatment and care for Covid-19, and points out the lack of information in public media on management of Covid symptoms at home and when to go to hospital. She clarifies the futility of the scramble for remdesivir and the call for plasma donations and reiterates the need for masking and vaccination. “Masks work very well,” she said. “We got through the first wave of the pandemic by sheer masking and social distancing. Masking has been found to be the best possible method to keep Covid infection at bay.” And needless to say, Indians celebrated the waning of the first wave a bit too early.
Excerpts of the rest of the discussion where she answers questions on treatment and home care.
Q/ People are running from pillar to post to find remdesivir. Doctors are asking for it, there is a black market, there are fake drugs. Is there scientific evidence that remdesivir works and at what point should it be used to save a life?
A/ One of the reasons why the crisis is so bad is because people going into the hospital think remdesivir is lifesaving and really it is not. The medical community needs to stand together and say that remdesivir is useless [during a surge like India's second wave]. Remdesivir has been shown to be mildly effective in the number of days that people shed the virus, in the trials conducted in the US and the UK. So, it reduces the number of days they need hospitalisation, but it has not been shown to reduce the risk of death. When a severely ill patient is gasping for breath, putting a patient on a bed on IV for a small potential benefit is criminal. You are taking the bed away from other patients and [preventing them] from getting lifesaving medication, getting oxygen.
The most important treatment for Covid when patients get to the hospital is oxygen and steroids. These are the treatments that are lifesaving. And going to the hospital to get remdesivir that does not help you much is stressing the system immensely.
Q/ What is your opinion on the use of tocilizumab?
A/ Tocilizumab as a medication should be given only in a hospital setting and has a very niche role. It is highly immunosuppressing and is only indicated to patients who are deteriorating, who are on a ventilator, not doing well. It is something that a medical professional who is treating you needs to decide after weighing the pros and cons. It is not something that probably 99.9 per cent of patients with Covid-19 would need.
Q/ Patients are being asked to do a CT scan. Are these useful to planning an efficient treatment protocol?
A/ In the US initially, we did CT scans on every patient since we did not know enough about the disease. But we have learnt from it. And the lesson we learnt is that the CT scan does not help in any way, there is no direct correlation between appearance on CT scan and outcome of the patient. What matters is the level of oxygen and so a simple pulse oximeter reading is much more valuable than a CT scan. Therefore, doing CT scans is useless for the patients, potentially harmful and is taking away valuable medical resources.
Q/ What about plasma donations? How effective is plasma therapy?
A/ Plasma does not work. Plasma is useless. Do not donate plasma, do not try to arrange for plasma. It is a waste of time and money and again it is stressing the medical system. Obtaining plasma, doing the testing on the plasma, administering the plasma, which is completely useless is taking that time and energy that should be devoted to patient care. I cannot emphasise that enough. I can say this confidently since the plasma trial was initiated in Mayo Clinic, a good friend of mine led the first plasma trial. The data shows that it does not really help. The only marginal benefit was for patients with lymphoma and those with long-term Covid effect. That too about one in three lakh cases.
Q/ What is your recommendation on budesonide inhalers or nebulisers?
A/ It is like remdesivir in that it has a mild benefit. If you use it early, it helps reduce the cough, so patients feel better and are less worried about progression. It also may help with reducing progression to avoid hospital stay. Budesonide is less expensive and can be administered at home. However, the data is limited. The study that showed that it worked is called the principle trial and there were 2,000 patients in each arm and the patients who got the budesonide were less likely to go to the hospital by 2 per cent. The reason we put it in the recommendation was because it is cheap, could be administered at home easily and because the number of cases [was] so huge, that 2 per cent reduction is still a significant number. But again, it is not a lifesaving drug. If you have it, you can use it, but if you can’t find it, do not worry.
Q/ What are your suggestions on what citizens can do to reduce the impact of the pandemic?
A/ Lockdown, even if it is a self-imposed one. Do not go out unless absolutely required. This will help in creating a dent in the infection rate. If you have not already been vaccinated, please do so. The vaccines that are available in India may not prevent infection, but they definitely reduce the risk of serious illness, hospitalisation and death. If going out is unavoidable, use masks. Masking significantly reduces [chances of] you getting the infection and passing it on to others. If you have symptoms of Covid—usually fever, sometimes loss of smell /taste, cough, body aches—please find testing if possible.
The only medications you need are really things like paracetamol to reduce your fever. Drink plenty of fluids. Most people who get infected with will recover without complications. A very small number of people will need to be in the hospital. If you are feeling well, please do not go to the hospital even if your test is positive because that will take away a bed from someone who really needs it.
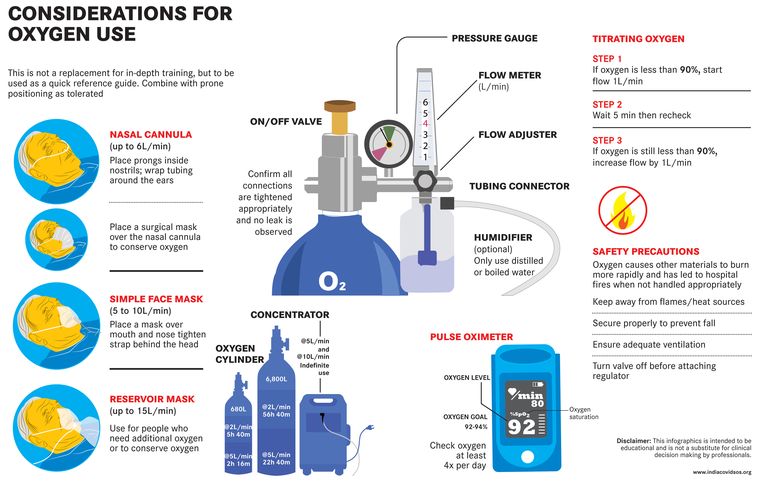
The one piece of equipment you should get to keep at home is the oxygen saturation meter. This measures the amount of oxygen in your blood and can be helpful in determining when you need to go to the hospital. If the oxygen percentage as detected by the meter is less than 92 per cent, that is the point at which you need oxygen and medication called dexamethasone or another kind of steroid. Even this can be done at home for many people, but if there is no possibility of arranging for oxygen at home and if hospital beds are available, this would be a good time to get admitted.
We do not need medications like remdesivir and tocilizumab. These are the medications for which people are going into the hospital. Do not get admitted to the hospital just to get these medications, unless your oxygen levels are going down.