The thyroid, a butterfly-shaped gland in the front of our neck, produces the hormones T4 (thyroxine) and T3 (triiodothyronine). These hormones are regulated by the thyroid stimulating hormone, which is synthesised by the pituitary gland (situated at the base of the brain). The thyroid hormones help in the regulation of fat, protein and glucose metabolism, modulating body temperature and maintaining overall equilibrium.
The often-discussed functions of the thyroid hormones are related to body weight, energy levels, cardiac fitness, digestion and gut motility, skin and hair quality, sleep and mental wellbeing, and sexual health, fertility and pregnancy. An important aspect which is often overlooked is their role in regulating bone health.
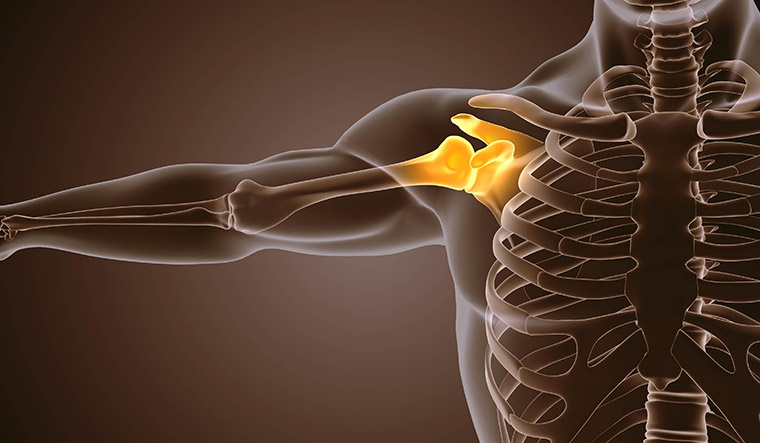
The thyroid hormones are essential for normal skeletal development and play an important role in the maintenance of bone structure and strength. The skeletal system is one of the largest systems of our body and its important components include structural proteins like collagen, minerals like calcium-phosphorous, and cells like osteoclasts (responsible for bone dissolution) and osteoblasts (responsible for bone formation and replacement). Any disturbance in thyroid hormone levels disrupt the balance of bone dissolution and replacement.
Therefore, bone health can be adversely affected in various states of thyroid dysfunction. Dysfunction can be excess functioning of thyroid hormones―hyperthyroidism―or under functioning―hypothyroidism. Both situations can have detrimental effects on musculoskeletal fitness.
Impact of hyperthyroidism: The activity of osteoclasts increase and there is rapid bone dissolution. The bone replacement by osteoblasts cannot match-up, leading to net bone loss. Additionally, in hyperthyroid individuals, there is more calcium loss via the urine and inefficient calcium absorption via the gut, leading to negative calcium balance. These factors eventually lead to low bone density and osteoporosis, a condition associated with fragile bones. Osteoporosis itself has no obvious symptoms, unless fracture occurs.
People with untreated hyperthyroidism have 12 per cent to 20 per cent reduction in bone density and three to four times increased risk of hip and spine fractures. This is more evident in the elderly and post-menopausal women. Even treated hyperthyroidism is known to have residual negative effect on bones―increasing the risk of fractures up to two times.
Impact of hypothyroidism: Reduced activity of the osteoclasts and osteoblasts lead to low bone turnover. The decreased bone metabolism affects children more than adults. Childhood hypothyroidism causes delayed skeletal development, impaired mineralisation of bones and slowing of normal growth. Delayed eruption of teeth, hip dislocation and abnormal curvature of the spine can be other manifestations in children. Congenital hypothyroidism in India varies from one in 750 to one in 2,500 newborns, depending on the geographical location.
In adults with hypothyroidism, the overall quality of bones may become poor with time, although, there is no direct correlation between osteoporosis and low thyroid hormones. Hypothyroidism often affects muscles, causing pain, cramps, weakness and lethargy, which, in turn, can lead to increased tendency to fall and fracture. Also, people with hypothyroidism on thyroxine treatment should have regular blood tests to ensure that their hormone levels are not too high, as it can lead to treatment-induced hyperthyroidism.
Bone care in patients with thyroid dysfunction: Early identification and proper treatment of thyroid dysfunction is important as the bone involvement can be asymptomatic in the initial stages.
People with typical symptoms-cluster, like unexplained weight loss, tremors, palpitations, heat intolerance, anxiety, nervousness and protruding eyes, should get evaluated for hyperthyroidism.
Those with weight gain, fatigue, lethargy, constipation, dry and brittle nails, hair fall, cold hands and feet, puffiness of the feet and infertility, should get assessed for hypothyroidism.
Those with goitre (a swelling at the front of the neck caused by an enlarged thyroid gland) or a strong family history of thyroid disorders should consult an endocrinologist or a physician for further evaluation.
Patients on treatment for thyroid disorders should comply with the medicines, and be regular with their tests and medical follow-ups. In hyperthyroid patients, apart from the prescribed treatment, general measures for fall-prevention should be followed. Regular physical activity, balance exercises and yoga, properly fitting and sturdy footwear, proper lighting of living spaces, especially bathrooms and hallways and use of assistive devices like handrails can go a long way to prevent falls.
High impact exercises like jogging and power-walking help strengthen bones and muscles.
Eating a well-balanced diet of calcium and protein rich food, maintaining normal vitamin D levels, and avoiding smoking and alcohol help keep the bones healthy. Supplements are recommended for populations where diet does not provide adequate calcium.
Adequate vitamin D production occurs from frequent, mid-day sun exposure―10 to 30 minutes for three to five days a week. However, repeated, long-duration exposure can cause sunburns, eye problems and heat strokes. It is thus easier to consume vitamin D supplements as per your doctor’s advice. Some patients with osteoporosis, especially elderly women, may also need specific anti-osteoporosis therapy.
Screening for thyroid dysfunction in each new-born should be done, so that thyroid insufficiency is identified at the earliest. Consult paediatricians regarding children with delayed growth, inappropriate weight gain, deteriorating scholastic performance, slower reaction time and sluggishness, irritability and constipation.
Maldar is consultant endocrinologist, P. D. Hinduja Hospital and Medical Research Centre, Mahim.