The autumn of 2014 gave sleepless nights to biologist Vasan Sambandamurthy. He and his two colleagues—Shahul Hameed, a medicinal chemist, and Dr Suresh Solapure, an expert in drug metabolism and pharmacokinetics—were awaiting a verdict that would make or break their career as researchers.
For four years, the three scientists had kept their noses to the grindstone at a laboratory in Bengaluru to come up with Compound 12, a molecule that had the potential to cure drug-resistant malaria. On September 26, they went to Switzerland to present it to a panel of experts at Medicine for Malaria Venture (MMV), a non-profit organisation that supports research and development of affordable antimalarial drugs. The panel’s feedback was critical in deciding whether the molecule was worth clinical trials.
The scientists desperately needed the approval. Their laboratory was on the verge of closure, and four years of their research was at stake. “Sleep eluded us that night,” said Solapure. “We were happy, yet anxious. The fear of failing at that stage was not unfounded.”
Finally, two months after their trip to Switzerland, the trio received the formal approval from MMV. Compound 12 could now enter clinical trials. The scientists celebrated by having their favourite ice cream.
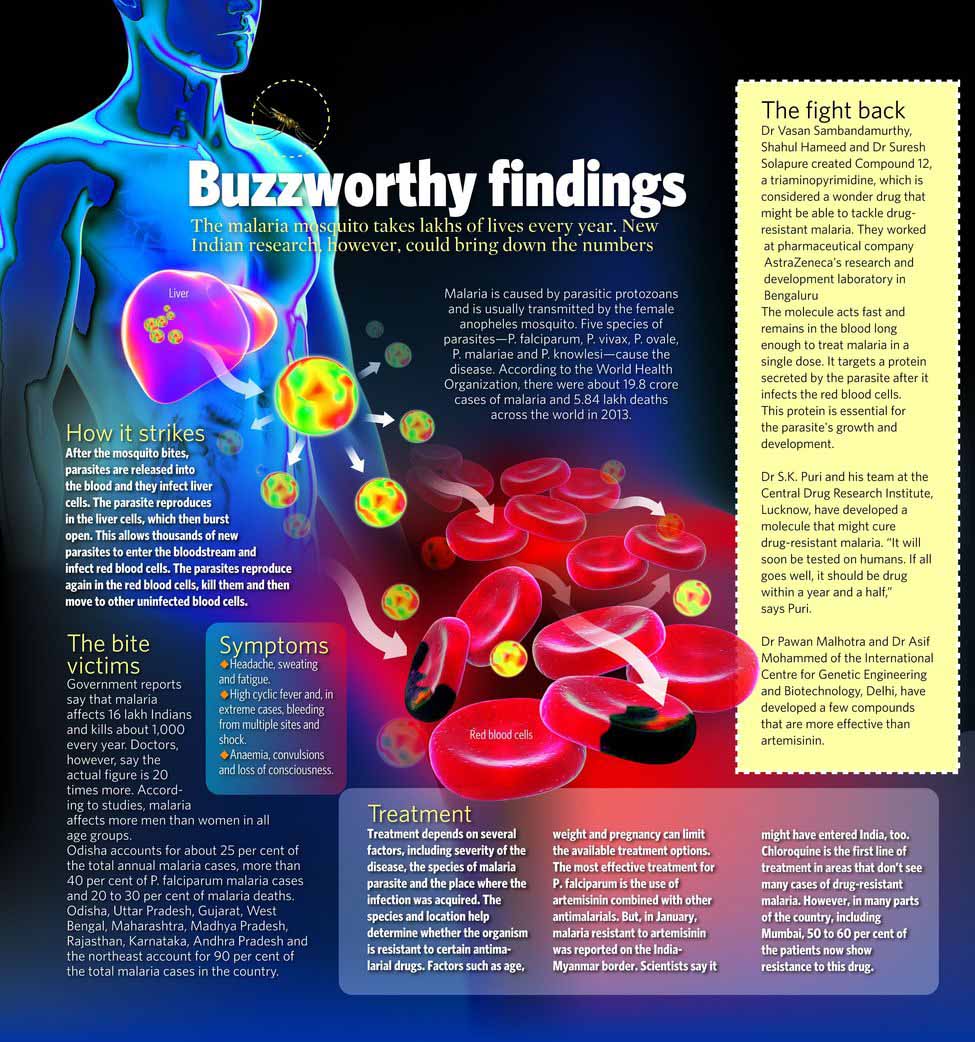
Compound 12 is a wonder molecule that could well win the battle against malaria, which puts three billion people at risk and kills five lakh every year. The malaria parasite is a cunning foe. Some of its strains have mutated and become resistant to every medicine developed to kill it.
Scientists first spotted the malaria parasite’s resistance to artemisinin derivatives, currently the most effective antimalarial drugs, in the Greater Mekong region of south Asia in 2008. Recently, the same multi-drug resistant strain was spotted along the India-Myanmar border.
Looming large is a drug-resistant malaria epidemic, with the potential to undermine 15 years of steady progress in the fight against the disease. “There is need for medicines that will interrupt the cycle of transmission between mosquito and man, treat relapsing malaria that is common in Asia, and protect some of the most vulnerable populations,” said Jaya Banerji of MMV.
Agreed Harsh Vardhan, Union minister for science and technology: “We need to revive the national malaria control programme in a big way. We need to strengthen our surveillance systems to rule out the possibility of spread of drug-resistant malaria.”
It took close to 12 years for chloroquine to become a drug of choice in the treatment of malaria after it was discovered by German scientist Hans Andersag in 1934. That is the kind of time it takes for a molecule to become a medicine. For more than 30 years, chloroquine was the only antimalarial available worldwide.
Scientists spotted malaria’s resistance to chloroquine in the 1960s. But the hunt for another potent antimalarial drug started only a decade later. As a result, malaria control programmes around the world suffered setbacks. In India, the disease, which was on the verge of being eradicated in the 1950s, came back with a bang in the 1970s. Government statistics showed a jump from a mere 5,000 cases in 1961 to 65,00,000 in 1976.
Till now, the country has not been able to eradicate malaria. The mosquito that spreads malaria, female anopheles, is getting ‘smarter’, and so are the two main strains of the malaria parasite—plasmodium falciparum and plasmodium vivax.
What helped in the 1970s was the development of derivatives of artemisinin, an ancient Chinese medicine. Till date, this group of drugs has been battling malaria across the globe. But the resistant strain of malaria parasite that was isolated in southeast Asia in 2008 shows that the disease has gone to the next level.
The need of the hour is a new cure. Scientists who are out to find it, however, face a host of challenges, ranging from lack of funds and political will to lack of interest of pharma companies to invest in research, as the margin from antimalarials is far less than that of drugs that battle lifestyle diseases.
In India, three independent teams of scientists have fought against all odds to develop molecules that could be turned into potent drugs against the resistant strain of the malaria parasite. Chief among them is the group led by Sambandamurthy, whose Compound 12 holds the most promise. Sambandamurthy and his colleagues started their research in the Bengaluru facility of pharma major AstraZeneca in September 2010. AstraZeneca was approached by MMV to undertake a project to find a cure for drug-resistant malaria. The research was done in collaboration with Eskitis, a laboratory in Australia that has one of the richest ‘libraries’ of molecules.
From more than two billion compounds at Eskitis, Hameed, the medicinal chemist in the team, selected five lakh compounds for their research. “It was like a dream destination for a chemist,” he said. “There were molecules from every possible chemical series. These molecules must have shown efficacy towards one or the other disease. It takes years of research to build this kind of a collection.”
The next step was to screen all five lakh molecules against the malaria parasite, and look for ones that could kill it. They used a high-tech robotic system called high throughput screening to do it. “The robot takes only a couple of weeks to screen the molecules, but we took four months to prepare for the screening,” said Hameed.
For the screening, the scientists cultured plasmodium falciparum and fed them human red blood cells. As the parasite grew, fresh red blood cells were given on a regular basis. The next step was to add the compound and wait for 48 hours to see its effect on the parasite growth.
“The compounds kill the parasite by targeting hundreds of protein arrangements that might be responsible for signalling, or a physiological response in the parasite. Then you find a mechanism by which the compound inhibits the pathway. To be able to do that, a compound has to gain entry into the parasite. So, the first challenge is to break this barrier,” said Hameed. “Once you achieve that, you have to optimise the molecule so that it hits only the parasite and not other cells. This is easier said than done. The process of optimisation takes anywhere between a year to a year and a half.”
After two years, the team found a molecule that seemed promising. But the excitement vanished when toxicology tests showed that the molecule had poor solubility and could affect the heart. “This was a regular affair in the lab. It takes months for a chemist to optimise a molecule, but it takes a few hours for a biologist to find its flaws,” said Hameed, with a laugh.
There were moments when they lost hope. Yet, the scientists did not give up. They exhausted their knowledge of chemistry and pharmacology to modify the compound in a way that it reduces its limitations and enhances its desirable properties. More than a thousand compounds were synthesised to identify one lead molecule with the required levels of potency, specificity and other necessary characteristics. That is how they singled out Compound 12, which is now on its way to becoming a drug.
“That was the first high moment in our research,” said Sambandamurthy. “We were sure of our molecule and its performance in the laboratory. All our efforts were monitored by experts from around the world—AstraZeneca, Harvard and other collaborators. The stakes were high, as huge money goes into taking research from one level to another.”
The initial success meant the scientists had to try it on animals. They employed a 'humanised mouse'—a mouse having an impaired immune system and transfused with human blood. So the mouse’s reaction to the molecules would be identical to that of humans. The humanised mouse had another advantage—it could be infected with the same strain of parasite that infects humans, adding to the accuracy of the experiment.
The results were promising, and they proceeded to the next stage: to compute the dose of the drug for humans, based on molecule levels in the blood of mice, rats and dogs. “It took us another few months to conclude that a single dose of 260mg of Compound 12 might be sufficient to maintain therapeutic blood concentration for four to five days,” said Solapure.
How is the drug different from the existing antimalarials? Sambandamurthy said the new drug targeted a protein secreted by the parasite after it infects red blood cells. This protein secretion is essential for the parasite’s growth and development inside the cell. Other antimalarials do not target this protein.
Scientists carried out various tests on over 1,900 plasmodium falciparum parasites isolated from patients across the world and on laboratory strains that displayed various levels of resistance to antimalarials. None of the parasites showed resistance to Compound 12. The molecule also cleared toxicity studies on rats and guinea pigs.
The time had come to showcase Compound 12 at an international forum. “We had to prove that our molecule was good and worth investing in. We went to Switzerland and presented our findings at MMV’s annual meet, where they critically analyse all the researches they support and choose the most promising one. Our findings were well received by experts from across the world. But, in the meantime, AstraZeneca made an announcement to close down their R&D centre in Bengaluru, our laboratory,” said Hameed.
The wait for the formal approval was agonising. “I clearly remember the day it came,” said Hameed. “We were at our respective workstations on different floors at AstraZeneca. It was around 2pm and I heard a blip in my mailbox. I opened it and found a letter from MMV. Our research was accepted and our molecule could be taken forward for clinical trial. That was the magic moment. I rushed to Dr Vasan and, together, we went to collect Dr Solapure. We celebrated that moment with our favourite ice cream.”
So, what next? “Our part is over,” said the trio in chorus. They are looking forward to seeing Compound 12 become a drug. And they are confident that it will happen soon.
A second front in the battle against drug-resistant malaria was opened by a team of scientists at the Central Drug Research Institute in Lucknow. The man who led the research is Dr S.K. Puri, whose vaulting ambition in life was to become a banker. In 1976, Puri cleared the banking entrance exam and interview, and accepted an appointment letter. As he waited to join the bank, he visited his close friend, a research fellow at CDRI. It was his first-ever trip outside Chandigarh, his hometown.
The spirit of scientific inquiry at CDRI had a deep impact on the young, impressionable Puri, a postgraduate in science. There and then, he decided to change the course of his career and applied for a PhD at the institute. He was selected within a few hours, after an interview with the director of the institute.
As a student, Puri assisted his supervisor in the research on amebiasis, a parasitic infection. Soon, following an upsurge in drug-resistant malaria cases, the government asked the institute to restart its research on the disease. The malaria parasite was fast becoming resistant to chloroquine, the most effective antimalarial available at that time.
To contribute to the research, Puri read through the literature on pharmacology and parasite physiology. “We would use a mice model to study parasite in blood, and a bird model to study parasite in liver. I used to go to Delhi to collect the parasite model from the National Centre for Disease Control, the only institute that had animal-testing facility. There we used to breed the parasite,” he said.
At that time, CDRI was collaborating with Walter Reed Army Institute of Research in the US. “The Americans wanted access to monkeys for their research. As there were no monkeys in the US, they wanted us to help them with their studies. As I had some experience in handling the parasite in animals, I was given the task of carrying out studies on monkeys,” said Puri.
Every morning, he would observe the effect of drugs he administered to monkeys the previous evening, make charts, study medical literature and record his observations. Soon, he became a master at analysing the behaviour of monkeys and the effect of drugs on them.
Scientists who have worked with Puri say that he can tell you the level of drug and its effect on the blood of a monkey by merely looking at its eyes. “Monkeys hate me, but I love them,” said Puri. “It hurts me when I give them medicines, but I know it is in the larger interest of medical science.”
Puri's most recent contribution is 4-aminoquinoline, a molecule that can cure drug-resistant malaria. It was developed in 2011 and is already in the preclinical trials stage. “It has shown excellent results in laboratory experiments as well as in animal studies. It will soon be tested on humans. If all goes well, it should be made into a drug within a year and a half,” he said.
4-aminoquinoline is not the only big discovery Puri and his team have made. In the past 35 years, the institute has come up with two potent antimalarials: an ether derivative of artemisinin in 1980 and a drug called elubaquine in 1997. Elubaquine is one of the few drugs that treat malaria when it is in its latent stage in liver. Primaquine, the only drug available before elubaquine, had severe side-effects. “Elubaquine was one of the finest medicines we developed,” said Puri. “My team was on cloud nine when this molecule was accepted by a leading pharma company. The drug hit the market and worked very well in patients. But primaquine was much cheaper than elubaquine, so the government preferred the first. The company soon decided against producing the drug. I still believe that Primaquine should be replaced by elubaquine.”
Puri, who went on to become the director of CDRI, is now retired. But he still frequents the institute. “The scientist in me will never retire,” he said. “I will follow my passion with my students as long as I could.”
As one of his students set a slide on the microscope for him to check the quality of a parasite colony she cultured, Dr Pawan Malhotra, senior scientist at the International Centre for Genetic Engineering and Biotechnology in Delhi, exclaimed: “You have done such a wonderful job!”
Malhotra still displays a child-like enthusiasm when he talks about fluorescent dye cultures. “You need a child’s inquisitiveness to be a scientist,” said Dr Asif Mohammed, Malhotra’s colleague. “You need it to overcome harsh moments. We, scientists, may lose our years of research and hard work in one night. Yet, we have to start again.”
The two scientists recently developed a string of antimalarial compounds in collaboration with National Science Laboratory in Pune. These compounds are more potent than artemisinin and have shown efficacy against drug-resistant parasites. “So far, the results are promising,” said Malhotra. “We are hopeful that the compounds might turn into medicines soon.”
The two scientists have also identified another set of antimalarial compounds, thanks to studies done in collaboration with Canada-based University Health Network and CIDAVA Innovations, and Lifecare Innovations in India. Some of these compounds have already been tested in animals.
The duo’s research focuses on understanding the basic physiology of the malaria parasite. “We study various stages in the life of the parasite and try to identify stages or chemicals they secrete, against which we can develop a drug. It is basic science. But you build your experiments on it,” said Malhotra.
They started their research almost a decade ago, by identifying the process of haemoglobin degradation and hemozoin formation, an essential pathway involved in the parasite’s development. In plain English, they identified the stage in the life of the parasite when two main antimalarials—chloroquine and artimisinin—work.
Then they identified potent compounds that kill the parasite. Their study was awarded the $1,00,000 ‘Malaria Box Challenge Grant’ of MMV. “I would continue my research on new medicines for malaria,” said Malhotra. “But the dream is to be able to develop an antimalaria vaccine, which could prevent the infection. A vaccine is the only way to control malaria in such a vast country.”







