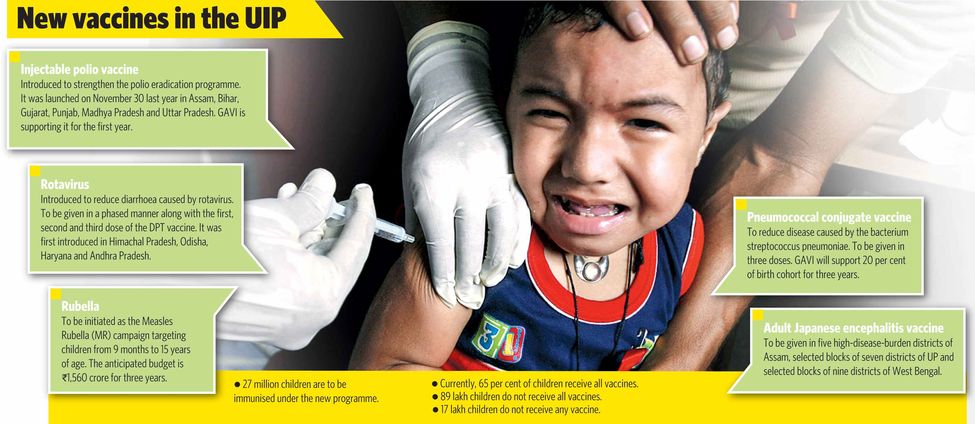
The ministry of health and family welfare has undertaken an ambitious expansion of its Universal Immunisation Programme (UIP) by introducing four new vaccines: injectable polio, rotavirus, rubella and pneumococcal conjugate. The ministry has also introduced a vaccine against Japanese encephalitis for adults in 27 districts where the disease is most rampant.
The initiative began with the introduction of the injectable polio vaccine (IPV) in six states last November. The IPV will soon be available across the country, along with the existing oral polio vaccine. In April, the health ministry will switch from the trivalent polio vaccine to the bivalent one to reduce cases of vaccine-induced polio.
New vaccines have been introduced to the UIP over the years; in 2010, it was measles and hepatitis; in December 2011, it was the pentavalent vaccine, which immunises against diphtheria, pertussis, tetanus, hepatitis B and haemophilus influenzae type b.
The recent expansion, however, is being viewed as one of the most significant government health initiatives of the past 30 years. Dr Rakesh Kumar, joint secretary, ministry of health and family welfare, says that the decision was taken after numerous scientific studies and comprehensive deliberations by the National Technical Advisory Group on Immunisation (NTAGI), the apex scientific advisory body on immunisation.
Some experts, however, believe that there is no rationale behind introducing so many new vaccines to the UIP as it will escalate health expenditure without significant results. "Nutritious food, potable drinking water, effective sanitation and hygiene would provide better protection against vaccine-preventable and other communicable diseases," says Dr Jacob Puliyel, paediatrician at St Stephen's Hospital, Delhi, and member of NTAGI. "The government needs to set its priorities right as far as allotment of money in the health sector is concerned."
Puliyel and other experts say that germs are only a part of the cause of a disease and that often there are many other important contributing, predisposing or determining factors. They believe there would be a marked decline in the prevalence of disease if there was an improvement in housing, sanitation, ventilation and personal hygiene. "We are falling prey to techno-centrism syndrome which is not good for the overall health of the country in the long run," says Dr Vikas Bajpai, professor, Centre for Social Medicine and Community Health, Jawaharlal Nehru University, Delhi.
To support his statement, Bajpai points out that from 1850 to 1965, England and Wales saw a 90 per cent decline in child mortality due to scarlet fever, diphtheria, whooping cough and measles. The first vaccine for diphtheria, however, was available only in the 1940s, the pertussis vaccine in the 1950s, and measles in the 1960s. Likewise, nearly half of the decline of smallpox occurred prior to the introduction of the WHO's smallpox eradication programme in 1966.
Scientists have also raised concerns about the adverse effect of vaccines. "Nobody is keeping track of vaccine-induced polio cases or many other similar paralytic diseases which are rampant in the country," says Puliyel. "Similarly, rotavirus causes a part of the total diarrhoea cases and the efficacy of the rotavirus vaccine is only around 50 per cent; 55 children have to be vaccinated in order to protect one child against diarrhoea caused by the virus, and the child will still not be protected against bacterial diarrhoea. There have been a few deaths reported following the administration of the pentavalent vaccine. In January, a two-month-old child died within 24 hours of administration of the vaccine in Ratnagiri district in Maharashtra."
Kumar, however, defends the government's move. "Rotavirus causes almost two lakh deaths every year," he says. "At any given point of time, at least 6 per cent of children suffer from diarrhoea; 50 per cent of this is caused by rotavirus. Death apart, diarrhoea results in morbidity and malnutrition in children. Though we are working on a health and hygiene campaign simultaneously, if vaccinations can save these children, it is worth it. It is easier to vaccinate them than to wait for them to understand the importance of hygiene and follow it. The rotavirus vaccine causes intussusception [an intestinal complication] in one in a million children and is treatable. It does have side effects, but that should not deter us from saving thousands of lives."
The ambitious programme—which aims to immunise 27 million children—faces several challenges, the biggest being the availability of adequate funds. Currently, GAVI, an international organisation, chips in. Eventually, however, the expenses will have to be borne by the government.






